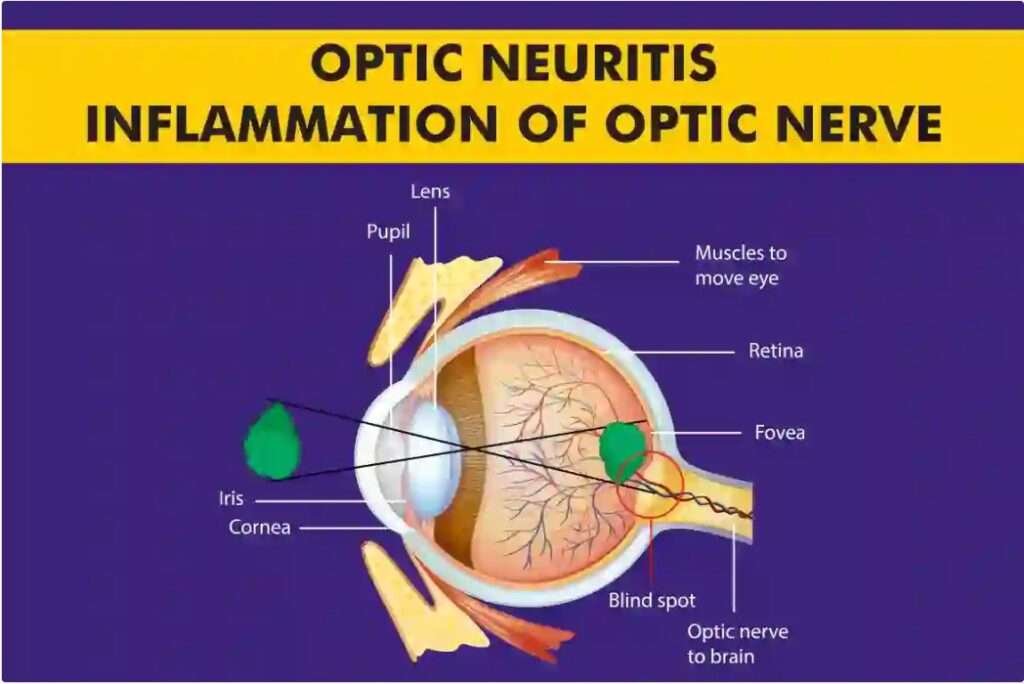
Optic neuritis (ON) is an inflammatory condition of the optic nerve that can lead to vision loss, eye pain, and other visual disturbances. This condition often serves as a clinical indicator of underlying systemic diseases, making its timely diagnosis and treatment crucial. In this blog, we explore the causes of optic neuritis and highlight the latest advancements in its management.
What is Optic Neuritis?
The optic nerve transmits visual information from the retina to the brain. In optic neuritis, inflammation damages the nerve, impairing its function. The condition commonly presents as sudden vision loss in one eye, accompanied by pain, particularly during eye movement. Other symptoms may include:
Loss of colour vision
Visual field defects
Reduced contrast sensitivity
Although optic neuritis often resolves spontaneously, untreated cases can result in permanent vision impairment.
Causes of Optic Neuritis
1. Demyelinating Diseases:
Multiple Sclerosis (MS): Optic neuritis is often the first manifestation of MS. The inflammation is linked to immune-mediated demyelination of the optic nerve.
Neuromyelitis Optica Spectrum Disorder (NMOSD): Associated with antibodies against aquaporin-4, NMOSD can cause severe and recurrent optic neuritis.
2. Infections:
Viral infections (e.g., herpes simplex, varicella-zoster, Epstein-Barr virus) and bacterial infections (e.g., Lyme disease, syphilis) can lead to optic neuritis.
3. Autoimmune Disorders:
Conditions such as systemic lupus erythematosus (SLE) and sarcoidosis can cause optic nerve inflammation.
4. Parainfectious Causes:
Post-viral or post-vaccination immune responses may trigger optic neuritis.
5. Toxic and Nutritional Factors:
Exposure to toxins like methanol and nutritional deficiencies, particularly vitamin B12 deficiency, can contribute to optic neuropathy.
Recent Treatment Options for Optic Neuritis
1. High-Dose Corticosteroids:
Intravenous Methylprednisolone: A standard first-line treatment, IV methylprednisolone accelerates visual recovery but does not influence long-term outcomes.
Oral Prednisone: Used in specific cases but associated with a higher risk of recurrent optic neuritis when compared to IV corticosteroids.
2. Plasma Exchange Therapy (PLEX):
Particularly effective in severe or corticosteroid-resistant cases, PLEX removes circulating autoantibodies and immune complexes, offering significant recovery potential.
3. Immunomodulatory Therapy:
For patients with recurrent optic neuritis or those linked to NMOSD or MS, long-term immunomodulation is critical. Common therapies include:
Interferon-β: Reduces relapse rates in MS-associated optic neuritis.
Rituximab: Effective in NMOSD by targeting CD20-positive B cells.
Eculizumab: Approved for NMOSD, it inhibits the complement cascade.
4. Neuroprotective Strategies:
Emerging treatments aim to protect the optic nerve from further damage. Research focuses on agents like:
Idebenone: An antioxidant shown to improve visual outcomes in some optic neuropathies.
Brimonidine: A topical agent under investigation for its neuroprotective effects.
5. Rehabilitation and Supportive Care:
Vision rehabilitation, including low-vision aids and therapy, is vital for patients with residual deficits. Counseling and psychological support are essential to address the emotional impact of vision loss.
Advancements in Diagnostic and Treatment Approaches
1. Biomarkers and Imaging:
Optical coherence tomography (OCT) provides detailed imaging of the optic nerve and retinal layers, enabling early diagnosis and monitoring of disease progression.
Serum biomarkers, such as anti-aquaporin-4 and anti-MOG (myelin oligodendrocyte glycoprotein) antibodies, aid in distinguishing NMOSD from other optic neuropathies.
2. Novel Therapies in Clinical Trials:
Stem Cell Therapy: Research into stem cell transplantation offers hope for nerve regeneration in optic neuritis.
Gene Therapy: Targeting specific genetic pathways to repair or replace damaged nerve tissues is an exciting avenue.
Conclusion
Optic neuritis is a multifactorial condition that requires a tailored approach to diagnosis and management. Advances in understanding the underlying mechanisms and the development of innovative treatments have improved outcomes for many patients. Early recognition and intervention remain key to preserving vision and preventing long-term complications. If you or a loved one experiences sudden vision changes or eye pain, seek prompt medical attention to ensure optimal care.